
The human brain is at the center of literally everything in life. Whether awake or asleep, the brain is constantly running, regulating every single process and function necessary for health and survival. But this delicate machine can be hijacked and sabotaged by drugs, with chemical compounds that can render the brain helpless and infected in a matter of minutes, and cause misery and suffering for years. The love-hate relationship between drugs and the brain is key to understanding how and why drugs work the way they do, and how treatment and therapy can undo the damage.
The Most Complex Structure in the Universe
 “The human brain is the most complex structure in the universe,” according to The Independent.[1] Much of that comes down to its intricate construction and composition of cells called neurons, which are informally referred to as nerves. Even the most simple and basic acts a human being can do, such as thinking (about anything), sensing something (e.g., temperature changes, aromas) and doing things, are the result of various neurons in the brain sending information to other neurons about what the respective thoughts, senses, or actions are. There are over 100 billion neurons in the brain, each single neuron connected to many thousands more.
“The human brain is the most complex structure in the universe,” according to The Independent.[1] Much of that comes down to its intricate construction and composition of cells called neurons, which are informally referred to as nerves. Even the most simple and basic acts a human being can do, such as thinking (about anything), sensing something (e.g., temperature changes, aromas) and doing things, are the result of various neurons in the brain sending information to other neurons about what the respective thoughts, senses, or actions are. There are over 100 billion neurons in the brain, each single neuron connected to many thousands more.
The brain does not work in isolation, and it is one of the two parts of the central nervous system, or the CNS (the other part is the spine). The CNS is responsible for most of the functioning of the body and the mind; while the brain is the machine that interprets information sent to it from other parts of the body, the central nervous system is the messenger that collects input from the body and then sends that information to the brain via the spinal cord. If the CNS were to be theoretically removed from the equation, the brain would be like a supercomputer that receives no data.[2]
While the brain and the spinal cord are the two parts of the central nervous system, the rest of the body is managed by the peripheral nervous system. The PNS is similar in form and function to the CNS in that it has its own neurons and nerves, and it overlaps with the CNS in some areas of regulating body movement and control. Because of this, scientists are looking at ways to address issues of pain without having to expose the brain and central nervous system to the risk of addiction. In 2012, for example, researchers at the University of California developed a chemical compound with a “completely new mechanism,” according to the lead investigator, which, in animal tests, proved effective. The drug bypassed the brain entirely, so the danger of having an addictive effect on the CNS was nullified. What the compound does instead is dull pain signals at their point of origin in the peripheral system; standard painkillers, on the other hand, target the CNS and the brain by shutting off all pain transmissions.[3]
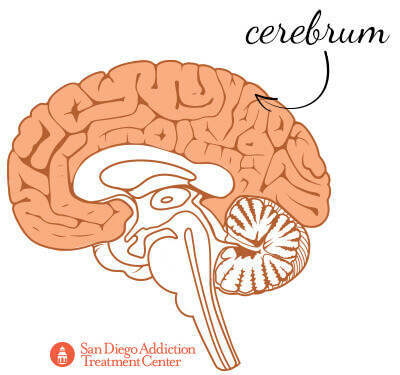
Inside the Brain: The Cerebrum
The brain has many parts to it, but the largest is the cerebrum, which is composed of the right and left hemispheres of the brain. The cerebrum is responsible for coordinating movement; regulating body temperature; and interpreting touch, vision, hearing, decision-making, problem-solving, emotions and learning.
The right and left hemispheres of the brain are connected by the corpus callosum (Latin for “tough body”), a mass of nerve tissues with over 200 million nerve fibers (called axons) that transmit electrical impulses between neurons. The corpus callosum is responsible for the two sides of the brain being in sync with each other. For people who are prone to seizures, surgical incisions into the corpus callosum isolate seizures and prevent the effects of a seizure from spreading into a healthier part of the brain.[4]
At the uppermost layers of the two hemispheres is the neocortex, which controls higher cognitive functions: spatial reasoning (drawing conclusions from limited information), conscious thought, language, and where motor commands are originated.
The neocortex is so important to human beings that it accounts for approximately 76 percent of the brain’s overall volume.[5]
The Cerebral Cortex and the Brainstem
The very outermost layer of the cerebrum is where the cerebral cortex is found, one of the most important parts of the brain. This is because the cortex is home to millions of neurons that, over time, form neural networks. The formation of neural networks is what learning is; it is how even the most instinctive and basic functions (like chewing and swallowing) are developed, so much so that, as adults, human beings don’t even give conscious thought to such activities.
Beneath the cerebrum is the limbic system, the structures of which (like the hippocampus, the amygdala, the hypothalamus and the thalamus) regulate both emotions and higher mental functions, like the formation of memory based on past experiences.[6]
At the base of the brain, and where the connection to the spinal cord (and the central nervous system) originates, is the brainstem, which is itself made up of three parts: the midbrain, the pons, and the medulla oblongata. The brainstem controls the transmission of messages from the brain to the rest of the body, and so it oversees the fundamental body functions, such as breathing, swallowing, blood pressure, consciousness, heart rate, and levels of wakefulness and sleep.[7]
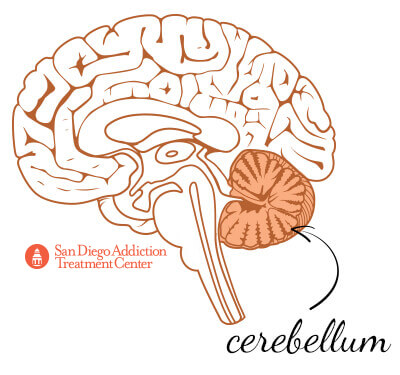
The Cerebellum and Neurons
Behind the brainstem is the second largest part of the brain, the cerebellum. This region is the one that specifically receives information from the body’s sensory system; based on this information, the regulation of motor movements begins in the cerebellum. Such movements can include posture, balance, speech, and coordination. The cerebellum ensures that all movements are harmonized, creating smooth and controlled muscular activity.[8] If the cerebellum is somehow damaged (from a traumatic brain injury, for example), a person could have difficulty maintaining balance or performing complex physical tasks.[9] The cerebellum contains approximately half of the brain’s neurons.
The brain is a perfectly balanced organ, with dozens of regions using hundreds of millions of chemicals to send messages and responses across the body within nanoseconds. Understanding the nature of this communication is key to seeing how drugs (both legal and illegal) can so easily rewire these vital components of the brain.
For example, consider neurons, which are made up of dendrites, a nucleus, and an axon. As neurons develop, the dendrites that receive information reach out and establish contact with the axons found at the end of neurons. This is the mechanism by which one neuron connects with another. The signals being communicated are either excitatory signals, telling the other neuron to become active, or inhibitory signals, telling the other neuron to stay passive.
Enter the Neurotransmitters
 There is no physical contact between two neurons; in fact, the space between them is important to the brain and how drugs derive their power once consumed. The space between the dendrites of one neuron and the axon of the next neuron is called a synapse. When the signal of an activated neuron reaches the synapse, a chemical messenger called a neurotransmitter is introduced into the equation. Neurotransmitters bridge the synaptic gap between neurons and fit with the receptors found on the dendrites of receiving neurons.
There is no physical contact between two neurons; in fact, the space between them is important to the brain and how drugs derive their power once consumed. The space between the dendrites of one neuron and the axon of the next neuron is called a synapse. When the signal of an activated neuron reaches the synapse, a chemical messenger called a neurotransmitter is introduced into the equation. Neurotransmitters bridge the synaptic gap between neurons and fit with the receptors found on the dendrites of receiving neurons.
The act of a neurotransmitter being a key that unlocks the receptor on the surface of dendrites is what makes a neuron either activated or inhibited. When its mission is accomplished, the neurotransmitters are reabsorbed into the axons, a process known as reuptake; this ensures that if a neuron needs to pass information to another neuron, the neurotransmitters are ready to be released into the synapse again.[10]
There are a number of different chemicals that can act as neurotransmitters, but just a few of them are responsible for most of the notable emotional, cognitive, and behavioral effects that people experience. These neurotransmitters are also the most susceptible to the influence of certain drugs because of how the chemical compositions of those drugs gives them the same kind of keys that unlock the connections between neurons. The drugs are engineered to be much stronger than the natural neurotransmitters, so the brain automatically defaults to the drugs, to the point where natural production of neurotransmitters does not have the same effect as those of the drugs.[11]
Dopamine, Adrenaline, and Serotonin
For example, the dopamine neurotransmitter regulates feelings of reward and pleasure (and the anticipation thereof), and it is drastically (and dangerously) targeted by any drug that affects how a user perceives being rewarded and pleasured. When talking about the love-hate relationship between drugs and the brain, dopamine is at the center of the conversation; anything from cocaine to marijuana, from opioids to amphetamine, influences the production and presence of the dopamine neurotransmitter, forcing neurons to stay activated for far longer (and with much more intensity) than normal. Stimulant drugs (such as cocaine, methamphetamine, or MDMA) also cause the overproduction of the norepinephrine neurotransmitter, which also regulates feelings of pleasure, alertness, and energy.
Adrenaline, also known as epinephrine, is a very well-known neurotransmitter, responsible for the “fight-or-flight” response in situations of extreme stress. Adrenergic drugs are given to patients who are unable to properly regulate how their body reacts in emergency situations; such substances possess similar chemical structures to the adrenaline that should normally be released during stress, interacting with receptors in the same way that adrenaline would, and stimulate the release of adrenaline in patients whose brains are unable to produce sufficient amounts of the neurotransmitter on their own.
Serotonin is a very important neurotransmitter that is used in the regulation of mood and impulsive behavior. Many different substances, from alcohol to stimulants, hallucinogens to antidepressants, influence the production (and can prevent the reuptake) of serotonin. For example, Mayo Clinic explains that selective serotonin reuptake inhibitors (SSRIs) are among the most commonly prescribed antidepressants in America because of their effectiveness in the treatment of depression.[12]
Scientific American adds to that, noting that doctors are prescribing SSRIs for a number of different conditions, such as:
- Attention deficit hyperactivity disorder
- Substance abuse
- Anxiety disorders
- Childhood autism
- Bipolar disorders[13]
Ready to leave substance abuse behind?
Call now to speak to a consultant about your treatment options
GABA and Acetylcholine

The GABA neurotransmitter is a critical chemical messenger that is secreted by the brain to regulate decision-making and impulsive behavior. According to the Current Pharmaceutical Design journal, GABA is the “major inhibitory neurotransmitter of the central nervous system.”[14] Chronic alcohol abuse has a direct impact on the GABA receptors because of the way ethanol mimics the effect of the neurotransmitters, which has the result of impeding the transmission between neurons. This is one reason why people who drink too much have difficulty making sound decisions and thinking clearly about acting in risky ways (such as driving while drunk or engaging in promiscuous or unprotected sexual behavior). Benzodiazepine drugs, a class of psychoactive medication, enhance the activity and increase the efficiency of GABA neurotransmitters, leading to greater inhibition and calming in patients.
For this reason, benzodiazepines are also prescribed for the treatment of:
- Insomnia
- Panic disorders
- Generalized anxiety disorder
- Sedation before surgery
- Seizures
Acetylcholine is an inhibitory neurotransmitter that regulates memory, motivation, and sleep, and it is vulnerable to the effects of a number of different kinds of drugs, like PCP and hallucinogens, as well as marijuana and stimulants. The journal of Neuropsychopharmacology, for example, looked into the “critical role of acetylcholine in the experience and progression of drug use,” and in particular the role of acetylcholine in cocaine dependence. Researchers noted that high levels of cocaine-driven acetylcholine in the hippocampus may even “encode” how the brain remembers and thinks about cocaine, all toward the eventual consumption of more of the drug.[15]
Similarly, Alcohol and Drug Research found that the most consistent effect of particular cannabinoids (including the primary psychoactive ingredient in marijuana) on animal subjects was to increase the secretion of acetylcholine in the hippocampus, having much the same effect as that of cocaine (albeit with significantly less potency).[16]
Endorphins
The last type of neurotransmitter to be most affected by the consumption of drugs is endorphins. Various parts of the body, such as the pituitary gland, the spinal cord, as well as the brain and the nervous system, produce endorphins as a response to stress, fear, or pain. When released, endorphins react with the receptors in neurons responsible for blocking pain and controlling emotions, such as pleasure. Exercise is an oft-cited example of endorphins at work; their release mitigates the physical discomfort of running or lifting weights and provides a surge of positive sensations. It is why exercise is widely recommended as a form of treatment for (and protection against) depression and where the idea of a “runner’s high” comes from.[17], [18]
Endorphins not only play a role in how a person perceives pleasure, but they are important in regulating those feelings; that is, the reuptake process of endorphins signals that the body and mind have had enough of the pleasure (which is why even highly rewarding activities, such as eating or sex, become undesirable after a point).[19]
Too Many Endorphins
Researchers have theorized that clinical depression, or unpredictable mood swings, might be partly the result of problems with either endorphin production or the binding process from one neuron to another. Similarly, for a person who has an imbalance of endorphins in the other direction (that is, a surplus of endorphins transmitting too many signals between neurons), the result could be unnaturally intense periods of anxiety or hypertension. People who suffer, witness, or otherwise experience a seriously stressful event undergo a deluge of endorphins (and other neurotransmitters), with the idea that the chemical messengers can assist with numbing the emotional and physical pain of the event. The more stressful the event, the more likely it is that the brain is unable to return to its default state, leaving those people in perpetual “flight-or-flight” mode; this is the mechanism by which post-traumatic stress disorder takes its toll. The Alcohol Research & Health journal notes that people who suffer from anxiety and depression in the aftermath of a traumatic event may use alcohol to cope because “drinking compensates for deficiencies in endorphin activity.”[20]
Endorphins and Opioid Receptors
 Endorphins interact with the opioid receptors in the brain to limit the perception of pain. In this way, endorphins have a similar effect as codeine or morphine, but without the potential for addiction.[21] The reason for this is that when endorphins bind to opioid receptors, the endorphins are quickly broken down by enzymes, allowing them to be reabsorbed for future use. Opiates (from prescription medication or heroin) have similar chemical shapes to endorphins, but they are notably different in structure. This means that they cannot be broken down by enzymes and instead keep the receptors activated for much longer periods of time than an endorphin neurotransmitter would. The result is that the person consuming the opiate feels a much stronger blast of euphoria and numbness than what endorphins are capable of producing, and this is what sows the seed of psychological and physical dependence.
Endorphins interact with the opioid receptors in the brain to limit the perception of pain. In this way, endorphins have a similar effect as codeine or morphine, but without the potential for addiction.[21] The reason for this is that when endorphins bind to opioid receptors, the endorphins are quickly broken down by enzymes, allowing them to be reabsorbed for future use. Opiates (from prescription medication or heroin) have similar chemical shapes to endorphins, but they are notably different in structure. This means that they cannot be broken down by enzymes and instead keep the receptors activated for much longer periods of time than an endorphin neurotransmitter would. The result is that the person consuming the opiate feels a much stronger blast of euphoria and numbness than what endorphins are capable of producing, and this is what sows the seed of psychological and physical dependence.
The way neurotransmitters bind to receptors has been called “a gateway to drug addiction,” and this is especially true of the mu opioid receptor. Current Opinion in Neurobiology explains that when this particular receptor is activated (from morphine administration or alcohol consumption, for example), a patient experiences positive reinforcement in the form of a powerful sedative feeling and the dulling of pain signals.[22] The Physiological Reviews journal further explains that the three kinds of opioid receptors (mu, delta, and kappa) are activated as a response to both “natural rewarding stimuli” (such as the release of endorphins during exercise), and “drugs of abuse.” The similarity is why users who consume drugs (such as the opioids that activate the three opioid receptors) not only feel good, but they feel rewarded as well. This makes the compulsion to seek out more drugs even stronger; and the more those receptors are exposed to the substances that hijack the rewards system, the stronger the addiction.[23]
Agonist Drugs
In the same way that there are different kinds of neurotransmitters, there are different categories of drugs (beyond opioids, stimulants, depressants, hallucinogens, etc.) that affect how neurotransmitters interact with their neurons.
Agonist drugs bind to specific receptors and cause those neurons to become more active. They boost the production of specific neurotransmitters, flooding the synaptic gap with more neurotransmitters than would normally be released. Therefore, more neurotransmitters bind with the receptors on the dendrites of the neighboring neuron, enhancing the original effect.
Agonist drugs can also prevent the reuptake of the neurotransmitter, which forces the neurotransmitter to remain in the synapse for longer than initially designed. This, in turn, forces the neurotransmitters to activate neuron receptors for longer than normal. When a person takes cocaine, for example, this is what happens to the norepinephrine and dopamine neurotransmitters.
Endorphins are examples of natural agonists; morphine and heroin are artificial opioid agonists. As explained above, artificial agonists bear such a striking similarity to the natural agonist that a receptor expects to bind with, that the receptor is effectively tricked into binding with the artificial agonist and then forced into a period of much stronger activation.
The Conversation likens natural agonists to master keys that fit locks (receptors) that open doors (activating a neuron).[24] However, drugs (artificial agonists) are copycat keys that work the same way for more nefarious purposes. Morphine is a good example; it mimics the structure of natural opioid agonists (specifically endorphins), so in the same way that people who exercise get a boost from their endorphins (which numb the pain of the exercise), people who receive morphine get a comparable boost (that also numbs pain), which is why morphine is used in the treatment of moderate to severe levels of pain.[25]
Likewise, tetrahydrocannabinol (THC, the main active ingredient in marijuana) is a cannabinoid agonist, activating the cannabinoid receptors in the brain. The body’s natural endocannabinoids normally do this, which help in the regulation of appetite, pain, mood, and memory.[26] People who have anxiety disorders have reduced levels of endocannabinoids, so the consumption of cannabis (with its THC) can alleviate feelings of depression and anxiety, or induce hunger in patients who have problems with their appetites.[27]
Antagonist Drugs
While agonist drugs boost the neurotransmitter signals working between two neurons, antagonist drugs impede the transmissions so the effects are diminished or even eliminated. They do this by fighting the neurotransmitter to bind to the receptors themselves; when they do, they effectively block the neurotransmitter from activating the neuron, so the neuron remains bound to the antagonist drug but dormant.
It is also possible for antagonist drugs to prevent neurotransmitters from being released into the synapse, rendering fewer neurotransmitters available to activate the target neuron.
A majority of the drugs that are abused recreationally tend to be agonists because they increase what neurotransmitters naturally do. Depressant drugs, like alcohol and benzodiazepines (sold as Xanax, Ativan, and Valium, among many others) are GABA agonists, helping the GABA neurotransmitter reduce more activity in neurons than it normally would (since GABA, as an inhibitory neurotransmitter, makes other neurons less likely to become activated).
As a depressant, alcohol slows down thinking, breathing, and heart rate by changing the levels of neurotransmitters in the brain.[28] Specifically, alcohol stops the excitatory neurotransmitters that would typically boost energy levels. But alcohol has the additional effect of increasing the inhibitory neurotransmitters, which typically calm activity.[29]
Amphetamines and Cocaine
 Stimulant drugs, on the other hand, primarily target the dopamine neurotransmitter. Amphetamines work in two ways: by inducing the terminals of dopamine-producing neurons to release more dopamine than normal, and by preventing the reuptake of dopamine from the synapse, resulting in the dopamine keeping the neurons active for much longer periods of time. For the norepinephrine neurotransmitter, amphetamine drugs act as agonists, competing with norepinephrine to reach receptors first and then keeping those receptors active.
Stimulant drugs, on the other hand, primarily target the dopamine neurotransmitter. Amphetamines work in two ways: by inducing the terminals of dopamine-producing neurons to release more dopamine than normal, and by preventing the reuptake of dopamine from the synapse, resulting in the dopamine keeping the neurons active for much longer periods of time. For the norepinephrine neurotransmitter, amphetamine drugs act as agonists, competing with norepinephrine to reach receptors first and then keeping those receptors active.
Similarly, cocaine blocks the reuptake of dopamine and serotonin. It only takes a few seconds for cocaine to enter the bloodstream and reach the brain, regardless of the manner of consumption (being snorted, smoked, or injected). Once in the brain, the overproduction of dopamine, and resultant stoppage of reuptake, causes the characteristically intense euphoric high. This is so unfathomably powerful that researchers have noted that lab animals, when given a choice between cocaine and food, will choose cocaine to the point where they starve to death.[30]
People addicted to cocaine have brains with “significant abnormalities,” which goes some way in explaining the compulsive behavior to seek out more cocaine (and then take dangerous risks while high), even as the evidence of deteriorating wellbeing mounts. Cocaine users experienced a “dramatic decrease in grey matter,” according to researchers at the Behavioral and Clinical Neuroscience Institute at the University of Cambridge. Grey matter contains the dendrites and axon terminals of neurons, so people whose brains were frequently exposed to cocaine suffered losses in decision-making, memory, and attention span. Notably, however, the rewards systems in those brains (found in the caudate nucleus region) was markedly enlarged than in normal brains.
The Hallmark of Cocaine
The Institute called this “the hallmark of cocaine dependence,” that even intelligent people will be driven to take significant risks to get more cocaine once they have been hooked.
Other areas of the brain tainted by cocaine included the insula, which regulates feedback processing and learning, and becomes active during periods of drug-related cravings.[31]
Researchers were quick to point out that despite their study showing the strong connection between cocaine and abnormal brain structures, the jury was still out as to the direction of the relationship. Are the abnormalities in the brain caused by cocaine, “or are people who have this abnormality more vulnerable” (to the impulse to use cocaine and then to demonstrate the typical effects)?
Regardless, the findings are encouraging for what they do show: that cocaine abuse “is a disorder of the brain” and not an issue of morality or willpower. The deeper understanding of what happens to the brain while under the influence of cocaine can help scientists and researchers devise ways to train and/or medicate the brain to compensate for the damage.[32]
It’s Not Too Late to Get Help for Addiction
Antagonist Drugs That Save Lives
Sometimes, the antagonist properties of certain drugs can be very useful. Opioid drugs work by binding to the opioid receptors in the brain (either the mu, kappa, sigma, delta, or gamma receptors), giving a person a boost of euphoria and a reduced perception of pain. One line of treatment for opioid overdose is naloxone, an opioid antagonist. Naloxone kicks other opioids off the receptors, thereby temporarily reversing the overdose.
For this reason, many police departments across the United States have outfitted their officers with a nasal spray-release version of naloxone, to revive people who have overdosed on opioids.
By January 2014, officers in Quincy, Massachusetts carried out this process 221 times and reversed 211 overdoses.[33]
Hallucinogens and Higher States
With hallucinogens (like LSD and MDMA), the mechanics of how the drugs work are similar, but the interactions are different. Rolling Stone magazine explains how brain imaging has revealed that any drug from this category causes “profound effects on neural activity,” some positive, some negative. Hallucinogens lead to less constrained brain functions, which can allow for better emotional regulation and increased creative expression. Such drugs also cause a tighter connection of various brain networks, leading some users to experience so-called “higher states of consciousness” and deeper levels of introspection.[34]
There are some things about this that the human brain is drawn to love. Limited studies have suggested that psychedelic drugs have notable potential in treating depression, post-traumatic stress disorder, anxiety, substance use disorders, and other mental health conditions. By increasing neural connectivity in some areas and decreasing brain functions in others, patients who take medically administered psychedelics can cope with their traumas or problems to potentially better degrees than via established pharmacological methods.
The Power of Psychedelics
 However, psychedelic drugs are nonetheless powerful, and some of them are infamous for the dangers they present. MDMA, for example, also known as Molly or ecstasy, is popular among fans in the rave and nightclub scene. MDMA stimulates the release of serotonin, dopamine, and norepinephrine, and also activates the release of oxytocin and prolactin hormones. The combination leaves users feeling the traditional euphoric rush and also contributes to users being incredibly uninhibited. Some users enjoy the feelings of emotional and sexual closeness, without actual sex; others use MDMA specifically to increase their sexual desires and then engage in sexual behavior with others. In both cases, the loud music, strobe lighting, and intense setting of the rave contributed to the euphoria and uninhibited states.[35]
However, psychedelic drugs are nonetheless powerful, and some of them are infamous for the dangers they present. MDMA, for example, also known as Molly or ecstasy, is popular among fans in the rave and nightclub scene. MDMA stimulates the release of serotonin, dopamine, and norepinephrine, and also activates the release of oxytocin and prolactin hormones. The combination leaves users feeling the traditional euphoric rush and also contributes to users being incredibly uninhibited. Some users enjoy the feelings of emotional and sexual closeness, without actual sex; others use MDMA specifically to increase their sexual desires and then engage in sexual behavior with others. In both cases, the loud music, strobe lighting, and intense setting of the rave contributed to the euphoria and uninhibited states.[35]
The downside is that the serotonin released by the MDMA consumption is in usually large quantities, which causes a deficiency in the brain. Users who go through this will feel depressed for days afterwards, which might compel the consumption of other drugs to try and self-medicate.
What Does Molly Do in the Brain?
Chronic MDMA use (generally categorized as moderate consumption every weekend for years at a time or significant consumption in a single weekend) can damage memory and learning. A 2013 study found that frequent MDMA users had lower activity in those regions of the brain compared to users who either rarely used MDMA or never used the drug at all.[36] Another study from 2006 found “neuropsychological evidence of frontal dysfunction” in MDMA users, specifically “widespread and marked verbal memory deficits.” Researchers published in the Journal of Psychopharmacology noted that MDMA users struggled with various aspects of learning, recalling information and recognizing past data they had been given. Scans revealed “a significant correlation between memory performance and the amount of MDMA taken.” The researchers concluded that impacts to the regions of the frontal cortex, as well as dysfunctions within the hippocampus, resulted in MDMA users suffering memory problems, which could last even years after the most recent consumption.[37]
Functional magnetic resonance imaging on the brain has furthermore shown that MDMA decreases activity in the amygdala and increases activity in the prefrontal cortex. The amygdala regulates threats and fear, so the reduction in activity correlates to users feeling more uninhibited and compelled into risky behavior, such as engaging in sexual activity with strangers. The prefrontal cortex, which is the brain’s center for higher thought processing, benefits from the MDMA in that users are less likely to be overwhelmed by anxiety and can better process their experiences, which may be useful for the treatment of post-traumatic stress disorder (a symptom of which is emotional numbness).[38]
Less Constraint, More Communication
 Additionally, recreational use of MDMA has been known to increase blood pressure, body temperature, and heartbeat to dangerous levels. Users report nausea, muscle tension, sweating, and chills. MDMA has been implicated in heart failure, kidney failure, and dehydration, and fatalities have been recorded for people who had health conditions that were exacerbated by the dehydration brought about by MDMA use in a loud, crowded environment.[39]
Additionally, recreational use of MDMA has been known to increase blood pressure, body temperature, and heartbeat to dangerous levels. Users report nausea, muscle tension, sweating, and chills. MDMA has been implicated in heart failure, kidney failure, and dehydration, and fatalities have been recorded for people who had health conditions that were exacerbated by the dehydration brought about by MDMA use in a loud, crowded environment.[39]
Other hallucinogens, like psilocybin mushrooms, have similar effects, such as increasing the chemical activity between parts of the brain that are normally disconnected from each other. Researchers at Imperial College London discovered, through functional magnetic resonance imaging scans of people who ingested psilocybin, that the connectivity patterns in their test subjects’ brains suggested “less constraint and more intercommunication.” A methodologist and physicist who worked on the study commented that the stronger connections create “a different state of consciousness,” similar to being in a very intense dream.[40]
Such results go back to the question of whether psychedelic substances can help patients with depression and anxiety disorders. The limited research done on the subject has offered results that suggest psilocybin can suppress unwanted brain activity, with the result that patients experience “a higher level of happiness and belonging to the world.” The Lancet journal ventured that psilocybin’s mood-elevating properties could be used in the treatment of addiction, obsessive-compulsive disorder, and post-traumatic stress disorder.[41]
But as with MDMA, concerns remain. Consumption of any kind of hallucinogen can lead to paranoia, or what Rolling Stone calls “a complete loss of subjective self-identity” (wherein users feel that they are “connected” with the objects around them and the universe at large, which can be disorientating and even dangerous if not handled correctly). The Imperial College London researchers cautioned that even the positive effects of hallucinogens can be uncontrollable, admitting that there is no comprehensive understanding of what psychedelics do to the brain.
Withdrawal, Treatment, and Recovery
Whatever the nature of a drug, the specific targeting of neurotransmitters that regulate feelings of pleasure, reward, and expectation is the mechanic behind addiction, particularly the difficulty and discomfort that arise when discontinuation is attempted. Withdrawing from a drug habit can be a traumatic and painful experience because the brain’s natural production of key neurotransmitters has been so long (and so powerfully) superseded by the drug that a person’s system is unable to produce enough of the chemical messengers. One of the most typical signs of withdrawal is a desperate craving for drugs, as the body struggles to naturally fill in the gaps that had, for so long, been amply filled by the boosted neurotransmitters.[42]
It can take a period of a few weeks (with professional supervision and careful administration of medication) for the withdrawal symptoms to subside and for the body to heal itself from the physiological effects of the drug use.
Neurotransmitter stocks are replenished, but the brain itself has to learn how to function without the presence of drugs. Counseling and rehabilitation play vital roles in teaching clients how they can avoid the pitfalls that led them to their drug use, and introduces new ways of thinking and coping with unfavorable situations, without the need for chemical substances. The process is not always easy, and there will likely be many bumps in the road, but with help, people can put down alcohol and drugs, and live happy and healthy lives.
Citations
[1] “The Human Brain Is the Most Complex Structure in The Universe. Let’s Do All We Can to Unravel Its Mysteries.” (April 2014). The Independent. Accessed March 7, 2017.
[2] “How the Spinal Cord Works.” (n.d.) Christopher & Dana Reeve Foundation. Accessed March 7, 2017.
[3] “Potential Pain Medication Targets Peripheral Nerves.” (September 2012). National Institute on Drug Abuse. Accessed March 7, 2017.
[4] “Corpus Callosum.” (April 2015). Healthline. Accessed March 8, 2017.
[5] “Neocortex (Brain).” (n.d.) Science Daily. Accessed March 7, 2017.
[6] “The Limbic System.” (September 2016). Boundless. Accessed March 8, 2017.
[7] “The Brainstem.” (September 2014). The Stroke Network. Accessed March 8, 2017.
[8] “Cerebellum.” (March 2015). Healthline. Accessed March 8, 2017.
[9] “Moving, Sensing, and Learning with Cerebellar Damage.” (August 2012). Current Opinion in Neurobiology. Accessed March 8, 2017.
[10] “How Drugs Affect the Brain.” (March 2016). MentalHelp.net. Accessed March 8, 2017.
[11] “The Brain from Top to Bottom.” (n.d.). McGill University. Accessed March 8, 2017.
[12] “Selective Serotonin Reuptake Inhibitors (SSRIs).” (June 2016). Mayo Clinic. Accessed March 8, 2017.
[13] “The Rise of All-Purpose Antidepressants.” (September 2014). Scientific American. Accessed March 8, 2017.
[14] Medications Acting on the GABA System in the Treatment of Alcoholic Patients.” (2010) Current Pharmaceutical Design. Accessed March 8, 2017.
[15] “The Role of Acetylcholine in Cocaine Addiction.” (April 2009). Neuropsychopharmacology. Accessed March 8, 2017.
[16] “Effects of Cannabinoids on Levels of Acetylcholine and Choline and on Turnover Rate of Acetylcholine in Various Regions of the Mouse Brain.” (1987) Alcohol and Drug Research. Accessed March 8, 2017.
[17] “Exercise and Depression.” (n.d.) WebMD. Accessed March 11, 2017.
[18] “Yes, Running Can Make You High.” (March 2008). The New York Times. Accessed March 11, 2017.
[19] “What Are Endorphins?” (October 2015). Everyday Health. Accessed March 9, 2017.
[20] “The Role of Uncontrollable Trauma in the Development of PTSD And Alcohol Addiction.” (1999). Alcohol Research & Health. Accessed March 9, 2017.
[21] “Endorphins: Natural Pain and Stress Fighters.” (n.d.) MedicineNet.com. Accessed March 9, 2017.
[22] “Mu Opioid Receptor: A Gateway to Drug Addiction.” (June 2004). Current Opinion in Neurobiology. Accessed March 9, 2017.
[23] “Reward Processing by the Opioid System in the Brain.” (June 2015). Physiological Review. Accessed March 9, 2017.
[24] “Explainer: How Do Drugs Work?” (April 2016). The Conversation. Accessed March 10, 2017.
[25] “Morphine.” (n.d.). WebMD. Accessed March 10, 2017.
[26] “Endocannabinoids.” (February 2015). Medscape. Accessed March 10, 2017.
[27] “Activating Cannabinoid Brain Receptors Could Replace Marijuana for Anxiety Treatment.” (December 2014). Medical News Today. Accessed March 10, 2017.
[28] “What Happens to Your Body and Brain When You Drink.” (April 2015). Business Insider. Accessed March 10, 2017.
[29] “What Alcohol Really Does to Your Brain.” (October 2012). Forbes. Accessed March 10, 2017.
[30] “The Neurobiology of Cocaine Addiction.” (December 2005). Addiction Science & Clinical Practice. Accessed March 10, 2017.
[31] “The Insula: A Critical Neural Substrate for Craving and Drug Seeking under Conflict and Risk.” (July 2014). Annals of the New York Academy of Sciences. Accessed March 10, 2017.
[32] “Cocaine Addiction Linked to Brain Abnormalities.” (June 2011). The Guardian. Accessed March 10, 2017.
[33] “Police Carry Special Drug to Reverse Heroin Overdoses.” (January 2014). USA Today. Accessed March 10, 2017.
[34] “What Psychedelics Really Do to Your Brain.” (March 2017). Rolling Stone. Accessed March 11, 2017.
[35] “MDMA and Sexual Behavior: Ecstasy Users’ Perceptions about Sexuality and Sexual Risk.” (2005). Substance Use & Misuse. Accessed March 11, 2017.
[36] “Verbal Memory Deficits Are Correlated with Prefrontal Hypometabolism in 18FDG PET of Recreational MDMA Users.” (April 2013). PLOS One. Accessed March 11, 2017.
[37] “Memory Deficits in Abstinent MDMA Ecstasy) Users: Neuropsychological Evidence of Frontal Dysfunction.” (May 2006). Journal of Psychopharmacology. Accessed March 11, 2017.
[38] “Numbness/Blankness of Mind: PTSD?” (2010). Psych Central. Accessed March 11, 2017.
[39] “Comedown – The Ecstasy Fallout.” (January 2002). The Guardian. Accessed March 11, 2017.
[40] “New Study Discovers Biological Basis for Magic Mushroom ‘Mind Expansion.’” (July 2014). Imperial College London. Accessed March 11, 2017.
[41] “Psilocybin with Psychological Support for Treatment-Resistant Depression: An Open-label Feasibility Study.” (May 2016). The Lancet. Accessed March 11, 2017.
[42] “Craving: When the Brain Remembers Drug Use.” (February 2010). Psychology Today. Accessed March 11, 2017.
Get Help Now.
Has addiction stolen your loved one? Take action and call (619) 577-4483 or fill out this form to speak with a Treatment Consultant about our drug rehab center or one of our facilities across the United States.
