
A look at the interface between insomnia and substance abuse reveals that these two conditions may or may not be causally connected, but are related in more than one way. As the Partnership for Drug-Free Kids explains, the link between insomnia and substance abuse is powerful but vulnerable to being overlooked.[1] According to the Partnership, the following highlights on insomnia and substance abuse shed some necessary light on the relationship between these two conditions:
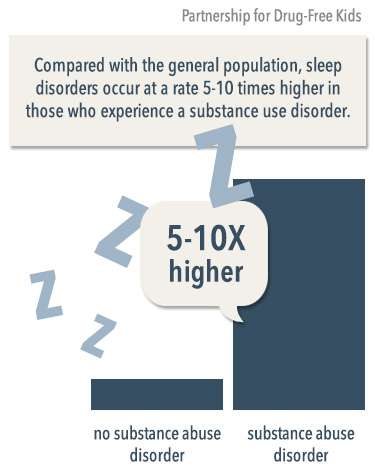
- Compared with the general population, sleep disorders occur at a rate 5-10 times higher in those who experience a substance use disorder.
- Alcohol dependence or other drug dependence can cause insomnia (and note, the insomnia persists even after abstinence is achieved).
- Sleep disorders can trigger relapse in those who are in recovery from abuse of a host of different drugs.
- Insomnia may be a risk factor for developing certain psychiatric disorders, including substance use disorders.
- Some individuals abuse sleep medications prescribed to them for relief of insomnia (and note, the insomnia may return after such persons are detoxed from the insomnia medications).[2]
As a discussion on the potential causal connection between insomnia and substance abuse would likely be more theoretically weighty than practical, the focus on the discussion herein is on the abuse of insomnia medications among persons with pre-existing sleep disorders. To provide the appropriate context to this discussion, this article first considers theories related to why humans need sleep as well as some of the risk factors present for insomnia. Even the briefest overview of insomnia reveals how sleep deprivation runs contrary to the most fundamental needs of the human operating system. When insomnia medication abuse is understood in the context of the experience of insomnia, it becomes clear how and why those who take these prescription drugs may become susceptible to abuse.
Important Information about Insomnia
It is well accepted across the world that a good night’s sleep is invaluable because of its restorative ability. The body and brain are quite busy while individuals sleep. According to the Division of Sleep at Harvard Medical School, while there is no definitive answer to why people need sleep, the following are some of the main ways in which sleep supports the survival and ongoing development of the human species:
- Known as brain plasticity theory, this approach focuses on how sleep pays an indispensable role in the brain development of infants and children, and the intelligent functioning of adults. Studies of adults show that a person who is deprived of sleep faces impaired learning ability. Undisturbed sleep in a constant time block (such as 7-8 hours) plays an instrumental role in the healthy functioning of complexes in the brain involved in memory. Research shows that memory underlies the ability to learn new information.
- In inactivity theory, the emphasis is on the fact that humans tend to sleep at night, which is a byproduct of an evolutionary necessity. Sleeping in the dark is thought to have served a key survival need, as humans would have been more vulnerable to predators if they hunted or gathered at night. In fact, sleeping at night may have given humans a genetic advantage over animals.
- Energy conservation theory is considered an extension or sub-theory of inactivity theory. This theory focuses on the fact that being asleep typically reduces energy metabolism by 10 percent. In short, if humans didn’t sleep, they would need more energy. This requirement would have been disadvantageous from an evolutionary perspective in view of reduced food availability earlier in human history when human genes were adapting to the environment.
- According to restorative theories, when a person is asleep, the body faces less competition for the lion’s share of the energy supply and can use this opportunity to repair the body. Support for this theory comes from findings that many of the main functions of the body (e.g., protein synthesis, tissue repair, and muscle development) occur when humans are asleep.[3]

In view of the many important brain and body functions that occur when we are sleeping, all of which may be an outgrowth of evolutionary necessity, the experience of insomnia appears all the more troubling. According to the National Sleep Foundation, insomnia is a health condition that covers problems falling asleep (i.e., sleep onset trouble) as well as staying asleep (i.e., sleep maintenance trouble).[4] While most every person in the world has likely experienced insomnia at some point in their lives, it becomes a chronic condition for some. The severity of a person’s sleep troubles is graded largely by its frequency and impact on daily functioning.
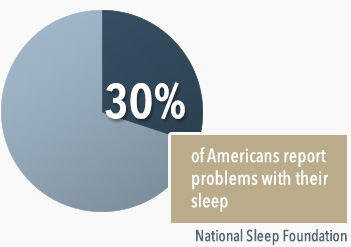
Acute insomnia is a brief experience that is usually triggered by an event or sudden emotional state. Persons are diagnosed with chronic insomnia disorder when they experience a disruption to their sleep for at least three nights per week over a minimum period of three months. According to the National Institutes of Health, an estimated 30 percent of Americans report problems with their sleep while approximately 10 percent experience mental and/or physical impairments in the daytime because of their sleep troubles.[5]
As Mayo Clinic notes, the following are some of the most common symptoms associated with insomnia:
- Daytime fatigue
- Inability to pay attention, remember tasks and information, and focus on tasks
- Depression
- Increased risk of making mistakes and greater susceptibility to accidents
- Anxiety
- Tension headaches
- Irritability
- A preoccupation with sleep, sleep troubles, and disruptive frustration
- Stomach/gastrointestinal tract problems
- Not feeling rested[6]
There are numerous risk factors for insomnia, including environmental and emotional ones. Stress can be a main or even sole contributor to acute or chronic insomnia. The most common stressors relate to the spheres of work, family, and school. An isolated event, such as a loved one’s death, illness in the family or personally, divorce, or being fired from work, can trigger sleeplessness. As Mayo Clinic discusses, the following are additional risk factors for insomnia:
- Sex status: Biological females are more likely than biological males to experience insomnia. For instance, female menstruation can cause sleep disturbances. Some women who are pregnant may experience insomnia.
- Age: The risk of experiencing insomnia increases with advancing age.
- Presence of a co-occurring mental health disorder: Anxiety, depression, post-traumatic stress disorder, and bipolar disorder (among other disorders) are known to cause sleep disturbances. For instance, early-morning awakening (an incomplete sleep cycle) is a well-known symptom of clinical depression.
- Work scheduling: Night work or having revolving work shifts that cross into or start at night can increase a person’s risk of insomnia.
- Jet lag: Those who travel across long distances into different time zones experience an increased risk of insomnia.[7]
Sleep disorders may be treated with therapy and medications. While prescription sleep medications can relieve the symptoms of insomnia, a fraction of prescribed users may develop an addiction to these pharmaceuticals. Unfortunately, the abuse of insomnia medications does not relieve the sleep disorder but rather summons the new health problem of addiction, which in turn requires treatment. A drug rehab center that offers a full continuum of care can treat the substance abuse issue as well as provide recovering persons with therapies that can help to manage the sleep disorder (which may persist after detoxification).
Insomnia Medications and Abuse Potential
According to the mental health clinician’s handbook, the Diagnostic and Statistical Manual of Mental Disorders – 5 (DSM-5), there are 10 disorders or disorder groups under the rubric of “Sleep-Wake Disorders.”[8] Insurance coverage for the treatment of insomnia typically requires an official diagnosis (i.e., the diagnosis is for one of the sleep-wake disorders officially recognized in DSM-5). When a person receives a diagnosis of a DSM-5 sleep-wake disorder, a doctor may recommend medications. At present, there is a general advisement that doctors screen patients with a history of substance abuse, or those who have substance abuse risk factors (such as a hereditary disposition), in order to stem the abuse potential of these drugs. The following are some of the most commonly prescribed generic and branded medications for the treatment of insomnia:

- Zaleplon (a branded drug is Sonata): Compared to other available insomnia medications, Sonata is active in the body for the shortest period; unlike Lunesta, there is little risk of next-day impairment. According to two studies, Sonata has an abuse potential that is similar to benzodiazepine/benzodiazepine-like hypnotic drugs.[9]
- Eszopiclone (a branded drug is Lunesta): Studies show that those who take this drug fall asleep rapidly and sleep an average of 7-8 hours. Lunesta has been associated with the risk of impairment the next day (i.e., it’s long-acting), and for this reason, people are usually started with a 1 mg dose. The manufacturers of Lunesta caution that those with a history of substance abuse may be vulnerable to abuse of this drug.[10]
- Zolpidem (includes branded drugs Ambien, Intermezzo, and Zolpimist): These medications have proven effective at inducing sleep as well as making it longer lasting.[11] According to research, zolpidem has significant abuse potential.[12]
- The benzodiazepine class (includes branded drugs with different generic bases such as Xanax, Restoril, and Halcion): These are older generation prescription sleep medications. These drugs tend to stay in the body system longer and have been effective in the treatment of sleep problems, such as night terrors and sleepwalking. These medications are associated with impaired ability in the daytime. Each of these medications carries an abuse potential.
- The antidepressant class of medications (includes branded drugs with different generic bases, such as Desyrel and Remeron): Crushing and then snorting Desyrel reportedly delivers a high that makes this drug a candidate for abuse. The makers of Remeron advise that while clinical trials of this drug did not reveal symptoms of abuse in participants, clinicians should screen patients for a history of drug abuse before prescribing this medication.[13]
- Doxepine (a branded drug is Silenor): Indicated for use in those who have problems remaining asleep. Silenor helps persons to maintain asleep, in part, by blocking histamine receptors. According to the manufacturer of Silenor, this medication has no risk for abuse.[14]
- Ramelteon (a branded drug is Rozerem): This medication targets the sleep-wake cycle without depression of the central nervous system, as do other insomnia medications. Rozerem is considered safe for long-term use. There is reportedly no evidence of Rozerem dependence or abuse.[15]
A review of the addiction potential of sleep medications necessitates consideration, from both the patient’s and doctor’s perspective, as to whether the benefits outweigh the potential risks. Sleep doctors interviewed by The New York Times advise that it is critical for a doctor to have a working theory as to the cause of the individual patient’s sleep trouble before providing a pharmacologically based treatment.[16] If use of a prescription sleep medication is warranted, it can difficult to gauge the true risk of abuse. The doctors report that in most instances the patients under their care who voluntarily increased their sleep medication dosage did so in the face of a stressful event that occurred after they were already on the medication.[17]
As there is no surefire way to determine a particular patient’s risk of abuse of a sleep medication, patient education and the prescribing doctor’s ongoing oversight are two potentially strong safeguards. The doctors interviewed noted that it is important for persons with sleep-wake disorders to be aware of alternatives to medication, as not all patients will necessarily need medications and can be helped with non-medication-based therapies.
Treatment for Insomnia Medication Abuse
The gold standard of substance abuse recovery treatment in a structured rehab program is to provide incoming clients with medically supervised detox followed immediately by intensive therapy. Typically, the safest way to detox from insomnia medications is to gradually wean off them rather than to suddenly terminate use altogether.[18] In the case of insomnia medication abuse, a person may be susceptible to relapse during the detoxification process because the insomnia may return. The supervision entailed in medical detox at a rehab center helps to ensure the recovering person will remain on the tapering plan. Once a recovering person is stabilized on a tapering schedule, the therapy component of the recovery program can begin (note, in some instances therapy can begin during the tapering phase).
Although those who abuse insomnia medications may appear to have a different type of abuse intention compared to those who abuse illicit street drugs, the same types of therapy can be used. Rehab centers typically offer recovering people both individual and group therapy. Individual therapy sessions can be tailored specifically to sleep medication abuse but usually serve as a gateway to the exploration of other factors. Individual therapy can help to address both the abuse behaviors around the insomnia medication as well as the potential causes underlying the insomnia in the first place.

The specific type of therapy approach that a therapist takes (or combination of approaches) depends on the rehab center’s overall treatment philosophy but will likely include research-based therapies. According to the National Institute on Drug Abuse, Cognitive Behavioral Therapy (CBT) is a research-based therapy that has gained considerable traction in the substance abuse treatment field.[19] The basic framework of CBT can be modified to the context of insomnia medication abuse. For instance, in CBT sessions, a therapist can work with a recovering person to identify the motivation for taking too much of a prescription insomnia medication. Once the thought processes that compelled this behavior are discovered, they can then be investigated with the purpose of being replaced by new and healthier coping strategies.
CBT can also be adapted to group therapy sessions. Most group therapy sessions are mixed in terms of the drug of abuse profile of participants. The logic here is that the particular drug of abuse is not as significant as the substance abuse behaviors that are usually common to all who have experienced addiction.
Depending on the rehab program, holistic treatments may be available (some programs refer to them as complementary or alternative treatments). Examples of holistic treatments include but are not limited to yoga, massage, meditation, and acupuncture. These forms of treatment are always intended to be supplemental to the two main recovery services (medical detox and intensive therapy). While these services are generally advisable, in the case of recovery from abuse of sleep medication, they are particularly recommended as a way of healthily managing the underlying sleep-wake disorder (which, again, may return after a recovering person begins detox/tapering off the medication).
Holistic Treatment of Sleep Disorders
According to the American Academy of Sleep Medicine, holistic treatments that center on relaxation techniques are advisable for those seeking help with insomnia. These techniques can involve exercises to relax muscles and deepen breathing, or visualization of one’s sleep goals/general peacefulness that is conducive to sleep.[20]
Holistic treatments may be vulnerable to stigmatization in mainstream society and remain a largely niche practice, even in light of the popularity of yoga in the US, which is mainly viewed as a form of exercise. To help combat imperfect perceptions of the use of holistic treatments for insomnia, as well as to offer sound scientific findings on this topic, researchers at Harvard Medical School and Johns Hopkins University School of Medicine conducted a related study. The researchers sought to learn about how insomnia sufferers use relaxation techniques and other holistic treatments as a method of self-help for this condition.
The researchers studied data initially collected by the National Health Interview Survey. The data reviewed covered a total of 23,358 adults. Of this group, 18 percent regularly experience insomnia or trouble sleeping in the past year. Of the insomnia sufferers, the demographics most represented were women, older persons, and individuals with lower education attainment and income levels. The researchers reviewed the entire group’s participation in the following types of holistic services:
- Yoga
- Tai chi
- Meditation
- Osteopathic treatments
- Chiropractic treatments
- Biofeedback
- Ayurvedic medicine
- Guided imagery
- Massage
- Acupuncture
- Non-vitamin and non-mineral supplements such as melatonin and valerian (marketed as natural sleep aids)
- Naturopathic treatments[21]
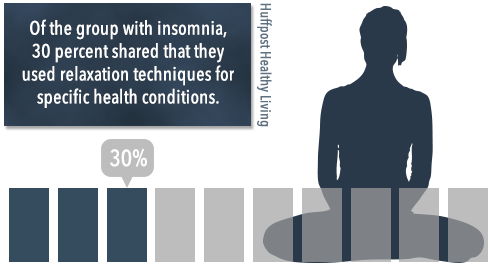
The researchers found that of the group with insomnia, 22.9 percent engaged in some form of relaxation therapy in the past year compared to 11.2 percent of those surveyed who did not have insomnia.[22] Of all forms of relaxation therapy, deep breathing was the most commonly used. Of all holistic treatments reviewed, the most popular type was natural pills, but they did not tend to be used in a way that addressed the insomnia in particular. Manipulative practices were second in popularity and included massage, osteopathic treatment, and chiropractic work.
Of the group with insomnia, 30 percent shared that they used relaxation techniques for specific health conditions. However, of this group, only 30 people reported the use of relaxation techniques specifically for their insomnia. These findings may have surprised the researchers. In sum, while it was true that those with insomnia were more likely than those without insomnia to engage holistic services, they did not do so to treat the insomnia per se. One explanation is that the general malaise that insomnia causes motivates individuals to engage wellness-oriented services; rather than deal with the sleep disorder, they try to improve the side effects, such as fatigue, sluggishness, poor digestive health, and depressed mood. Overall, the researchers appear to have considered their findings evidence that many with insomnia are missing an opportunity to use holistic treatments as a targeted approach to sleep-wake disorder relief.
Note that this research was not conducted in the context of drug recovery programs. An added benefit of seeking recovery services in a structured drug treatment rehab programs is exposure to holistic therapies. One reason Americans do not readily appear to engage holistic services is that they simply have not had sufficient exposure to them. Further, as drug recovery services help a recovering person to own their healing process, holistic treatment is a form of self-help that can conveniently be engaged in nearly any locale through a licensed provider such as a naturopathic doctor and/or self-directed activity like yoga and meditation. Those with ongoing insomnia after completion of a rehab program who engage in holistic treatments and experience an improvement in their sleep troubles receive all the proof they need. These individuals also have an added incentive to engage in alternative approaches as the earlier medication approach proved to be incompatible with their best interests.
Citations
[1] Vimont, C. (July 26, 2013). “Sleep Problems and Substance Use Disorders: An Often Overlooked Link.” Partnership for Drug-Free Kids. Accessed Dec. 9, 2015.
[2]Ibid
[3] “Why Do We Sleep Anyway?” (n.d.). Harvard Medical School, Division of Sleep. Accessed Dec. 9, 2015.
[4] “What is Insomnia?” (n.d.). National Sleep Foundation. Accessed Dec. 9, 2015.
[5] Ibid.
[6] “Insomnia: Symptoms.” (Apr. 4, 2014). Mayo Clinic. Accessed Dec. 9, 2015.
[7]“Insomnia: Risk Factors.” (Apr. 4, 2014). Mayo Clinic. Accessed Dec. 9, 2015.
[8]“DSM Library: Sleep-Wake Disorders.” (n.d.). American Psychiatric Association. Accessed Dec. 9, 2015.
[9]“Sonata.” (n.d.). Drugs.com. Accessed Dec. 9, 2015.
[10] “What is Lunesta?” (n.d.). Drugs.com. Accessed Dec. 9, 2015.
[11] “Drugs to Treat Insomnia.” (n.d.). WebMD. Accessed Dec. 9, 2015.
[12] Victorri-Vigneau, C. (Aug. 2007). “Evidence of zolpidem abuse and dependence: results of the French Centre for Evaluation and Information on Pharmacodependence (CEIP) network survey.” Journal of Clinical Pharmacology. Accessed Dec. 9, 2015.
[13] “Remeron.” (n.d.). Daily Med. Accessed Dec. 9, 2015.
[14] “Why Silenor?” (n.d.). Pernix Therapeutics. Accessed Dec. 9, 2015.
[15] “Drugs to Treat Insomnia.” WebMD.
[16] “Are Sleeping Pills Addictive?” (July 16, 2010). The New York Times. Accessed Dec. 9, 2015.
[17] Ibid.
[18] “Using medication: What can help when trying to stop taking sleeping pills and sedatives?” (Nov. 6, 2013). PubMed Health. Accessed Dec. 9, 2015.
[19] “Principles of Drug Addiction Treatment: A Research-Based Guide (Third Edition).” (Dec. 2012). National Institute on Drug Abuse. Accessed Dec. 9, 2015.
[20] Breus, M. (Jan. 28, 2013). “Can’t Sleep? Drug-Free Alternatives That Really Help.” Huffpost Healthy Living. Accessed Dec. 9, 2015.
[21] Ibid.
[22] Ibid.
